Integrated Traditional & Western Medicine: Managing Irritable Bowel Syndrome Effectively
Integrated Traditional & Western Medicine
Managing Irritable Bowel Syndrome Effectively
By Angela Carroll Adv. Dip. H.Sc. (Nat.), Adv. Dip. H.Sc. (Acu.), Adv. Dip. H.M.
IBS – A pain in the proverbial!
It is highly likely that a reasonable percentage of your patients are spending a lot more time in the toilet than is healthy. Irritable Bowel Syndrome (IBS) affects 15-25% of the population in Western countries, however IBS is often unrecognised or untreated, with as few as 25% of IBS sufferers seeking professional health care.
IBS is a chronic, episodic functional gastrointestinal (GI) disorder characterised by abdominal pain/discomfort and altered bowel habit (constipation, diarrhoea or alternating periods of both). Patients often experience additional symptoms such as bloating, sensation of incomplete evacuation, straining and/or urgency. IBS patients can experience symptoms for many years and those seeking care are often frustrated by the lack of effectiveness of conventional medical treatment. In this article we will look at the pathophysiology and drivers of this condition, as well as clinically effective management strategies for this common condition.
Addressing the drivers
In a study of 1620 people, 25% of which had IBS symptoms, more subjects with Irritable Bowel Syndrome had constipation and diarrhoea and 35% of patients with the syndrome reported rectal bleeding compared with an overall prevalence of 20%. Other symptoms and signs the IBS patients experienced included heartburn, dyspepsia, flushing, palpitations, migraine and urinary symptoms – interestingly these are all heat conditions. A history of abdominal pain in childhood was also more common in the subjects with IBS (12%). So where does all this heat come from? Modern research shows IBS to have 3 major drivers:
- Stress,
- Infection, and
- Food allergies.
It is these three drivers that result in the heat signs and symptoms. So let's look at each of these and review research conducted on TCM herbal formulas and how we can use them in the management of these key drivers of IBS.
Stress is the root of all evil
Stress and anxiety affect gastrointestinal tract (GIT) function in many ways (see Table 1).
All of the alterations, seen in Table 1, result in the symptom pattern commonly placed under the umbrella term 'IBS'. Interestingly, it appears that IBS patients have a disordered response to stress. In a study measuring the reactivity of the bowel to stress, researchers found that colonic motility showed a significant increase in the IBS patients during times of stress, compared with that of controls. Motilin, a hormone secreted in the small intestine which stimulates peristalsis, also increased significantly in IBS patients after stress. These phenomena are thought to be due to autonomic nervous dysfunction and/or gastrointestinal hormonal derangements induced by psychological stress. Other researchers have noted IBS patients also report higher ratings of stress, anger, and anxiety during the experimental stress compared with controls, who had smaller and nonsignificant subjective responses.
Coptis and Scute Combination (Huang lian jie du tang) has been traditionally used for clearing Damp-Heat conditions and used for patients with gastritis and intestinal inflammation. As stress is a major driver of intestinal inflammation, Coptis and Scute Combination was studied to see its effect on stress-induced gastric mucosal lesions. The study found simultaneous administration of the herbal formula with the stress exerted a preventative effect on the development of stress-induced acute gastric lesions in rats. This formulation may, therefore, be useful in your IBS patients to prevent GIT disturbances during times of stress.
|
Table 1. - Effects of physical, psychological and emotional stress on the GIT. |
|
Altered gut motility Increased transit time Decreased secretion of hydrochloric acid Decreased secretion of pancreatic enzymes Decreased secretion of bile Altered immune function with decreased resistance to infections and increased susceptibility to allergies Reduced gut wall integrity and development of “leaky gut” Predisposition to unfavourable gut flora – “dysbiosis” Increased inflammation of the gut wall and GI nerves Altered gut neurotransmitter levels and function |
Often medical management of IBS includes anti-anxiety medications and antidepressants, reducing the individual's response to stress. Modulation of this upregulated sympathetic nervous system response, (i.e. Liver Qi Stagnation) is also one of the most effective management approaches taken by TCM Practitioners, so the use of many of the TCM formulas to move Liver Qi Stagnation should always be part of IBS treatment.
It is also important that as Healthcare Practitioners we aware of the fact that psychological and/or physical stress may disrupt the normal balance of intestinal microflora. This induces dysbiosis then predisposes the individual to other drivers of IBS: infection and food allergies.
Infection adds insult to injury
Our body is constantly challenged by pathogenic organisms such as bacteria, fungi and viruses. These pathogenic organisms trigger numerous signaling pathways that ultimately lead to drastic changes in physiological functions. This includes potential induction of the local inflammatory response in the GIT.
Studies in animal models now clearly demonstrate a causal relationship between the presence of mucosal inflammation and altered sensory-motor function. Disturbances of motor function may produce a range of symptoms associated with IBS. Unfortunately for many IBS sufferers this disordered state may persist after the mucosal infection and inflammation has subsided; this state may be maintained by locally produced inflammatory mediators.
As we saw previously, Coptis and Scute Combination reduced stress-induced lesions; it has also been shown to reduce inflammation in the bowel. Research results indicate the formula is effective in the treatment of inflammatory bowel disease, showing a quickened healing process and a reduction of inflammatory cell infiltration following oral administration; effectively reducing interleukins (IL-8), leucotrienes (LTB4) and prostaglandins (PGE2).
Another TCM formula that has been found to significantly reduce PGE2 in the colonic mucosa is Pinellia Combination (Ban xia xie xin tang). This has the effect of promoting colonic water absorption. As a herbal formula that has traditionally been used to prevent diarrhoea, some of the anti-diarrhoeal effect may be due to the repression of PGE2 and the promotion of the water absorption capacity of the colon.
Inflammation and lesions within the mucosa may increase the pain often seen in IBS. A formula traditionally given to reduce abdominal pain is Bupleurum and Zhi Shi Formula (Si ni san). In a rat model, gastric lesions were induced chemically. In those post-administered Bupleurum and Zhi Shi Formula, all observed histological changes found were attenuated. The researchers concluded these results indicate that the herbal formula prevents the progression of gastric mucosal lesions possibly by blocking enhanced neutrophil infiltration, and by reducing destruction of the defensive barrier in the gastric mucosa.
Our body's natural anti-inflammatory, anti-stress hormone is cortisol. Oral administration of Pinellia Combination (Ban Xia Xie Xin Tang) caused a significant increase in blood cortisol levels and inhibited castor-oil induced diarrhoea. An inhibitory effect on cyclooxygenase-2 (COX-2) was also observed. The present results indicated that Scutellariae radix, Glycyrrhizae radix, Ginseng radix and Coptidis rhizoma-derived components are involved in the antidiarrhoeal action of Pinellia Combination.
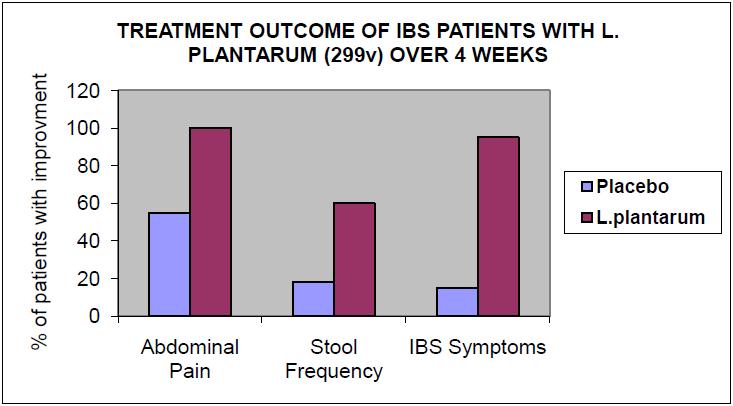
Figure 1: Lactobacillus plantarum 299v in IBS
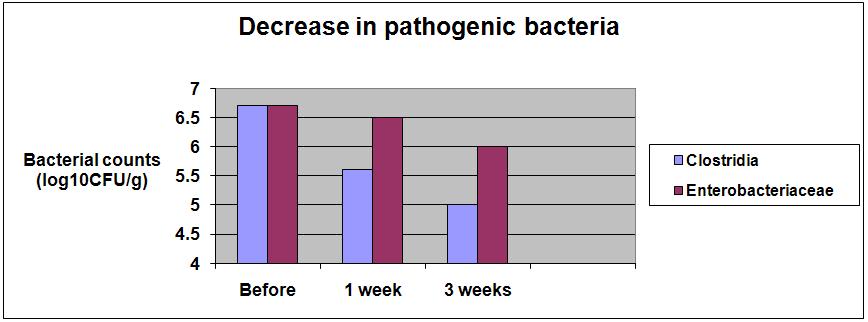
Figure 2: In those receiving L. plantarum 299v, a rapid reduction in sulphite-reducing Clostridia was observed within one week.
Gut flora – choosing the right strain for the job
Chronic bowel disturbances resembling IBS develop in approximately 25% of patients after an episode of infectious diarrhoea. Increased inflammatory cell numbers in the rectum persist for at least three months after the acute infection. Reducing inflammation in the GIT should always be a primary management solution for our IBS patients. Rebalancing a healthy gut flora is a first step in this process and utilising specific strains of anti-inflammatory flora has been found to have profound effects on reducing the pain, stool frequency and other IBS symptoms.
For example, in a double blind randomised placebo controlled trial of 40 patients with IBS, 20 were given Lactobacillus plantarum 299v and the remaining 20 were given a placebo. All patients taking the L. plantarum 299v had resolution of their abdominal pain with improvements in stool frequency and other IBS symptoms. (See Figure 1).
L. plantarum has demonstrated benefit in maintaining health of the digestive system by influencing the balance of micro-flora in the intestines and preventing infection. L. plantarum 299v has also been shown to possess anti-microbial activity against potentially pathogenic species such as Listeria monocytogenes, Bacillus cereus, E. coli, Yersinia enterocolitica, Citrobacter freundii, Enterobacter cloacae and Enterococcus faecalis in vitro (see Figure 2). L. plantarum 299v has also been shown to decrease the amount of gram-negative anaerobes and sulphite-reducing clostridia in rats and humans. , Gram-negative bacteria contain endotoxins that initiate violent inflammatory reactions within the intestine.
Food allergies: a hidden driver
The final driver that may contribute to IBS symptoms in your patients are food allergies. The evidence for immunological involvement in IBS is increasing: for example, abdominal pain has been found to correlate with activated mast cells adjacent to colonic enteric nerves. Given that mast cells are secreted in response to allergen exposure, this may indicate that food allergies play a role in the aetiology of IBS.
There is substantial evidence that enteric infections and inflammation result in “leaky gut” (i.e.: increased intestinal permeability), tending to increase the amount of antigens penetrating the intestinal mucosa, influencing sensitisation rather than tolerance to the antigen. This directs the immune response toward allergy in susceptible individuals. Additionally, it is known that infection and inflammation switch the dendritic cell from a toleragenic to a reactive, allergic state. Fortunately, TCM can help here too.
Three hours after a single dose of the anti-inflammatory Minor Bupleurum Combination was administered orally there was significant inhibition of histamine release in peritoneal cells in rats administered a strong allergen. This shows that Minor Bupleurum Combination has an active anti-allergic effect. The authors suggest that the formula inhibits Immunoglobulin (IgE) receptor-associated protein phosphorylation in the histamine release pathway.
Administration of formulas that reduce allergic reactions (See Sun Ten Newsletter September/October 2006) along with eliminating potentially reactive foods is an effective means of reducing IBS symptomology induced by food allergens.
Additional symptom relief
Here I wish to make mention of two more TCM formulas worth considering for reducing IBS symptoms. The first is Ren shen tang / Li zhong tang which has been found to significantly reduce small intestine contractions and improve small intestinal movement. This effect is attributed to the dried ginger root and ginseng in the formula. It is also thought that the mechanisms mainly involve the direct inhibition of smooth muscle but with a contribution from neural inhibition.
The second addresses the intestinal bloating so commonly seen in IBS: Pinellia and Magnolia Combination (Ban xia hou po tang). In patients with bowel gas volume significantly higher than that in healthy subjects the formula was administered for two weeks and resulted in a significant decrease in gas volume measured by plain abdominal radiogram. Furthermore, gastrointestinal symptoms, especially symptoms of abdominal pain, indigestion and constipation, all of which are closely related to abdominal bloating, improved significantly in these patients after the administration of Pinellia and Magnolia Combination.
Putting it all together
When patients present with IBS in your clinic, you have the ability to significantly reduce their symptoms and, if the drivers are successfully addressed, remission of the condition is easily achieved. Reduce the biggest driver – stress (Liver Qi Stagnation), and reduce the inflammation using both an anti-inflammatory formula and an anti-inflammatory probiotic like L. plantarum 299v. Finally, don't forget to eliminate reactive foods and, if you feel there is an allergy involved, use an appropriate formulation for managing allergies.
*Reproduced with kind permission from Health World Limited – Australia and New Zealand